From The Desk of

Matt dives into a specific healthcare topic to help those in the industry, and those outside of it, better understand the market drivers causing today’s healthcare challenges.
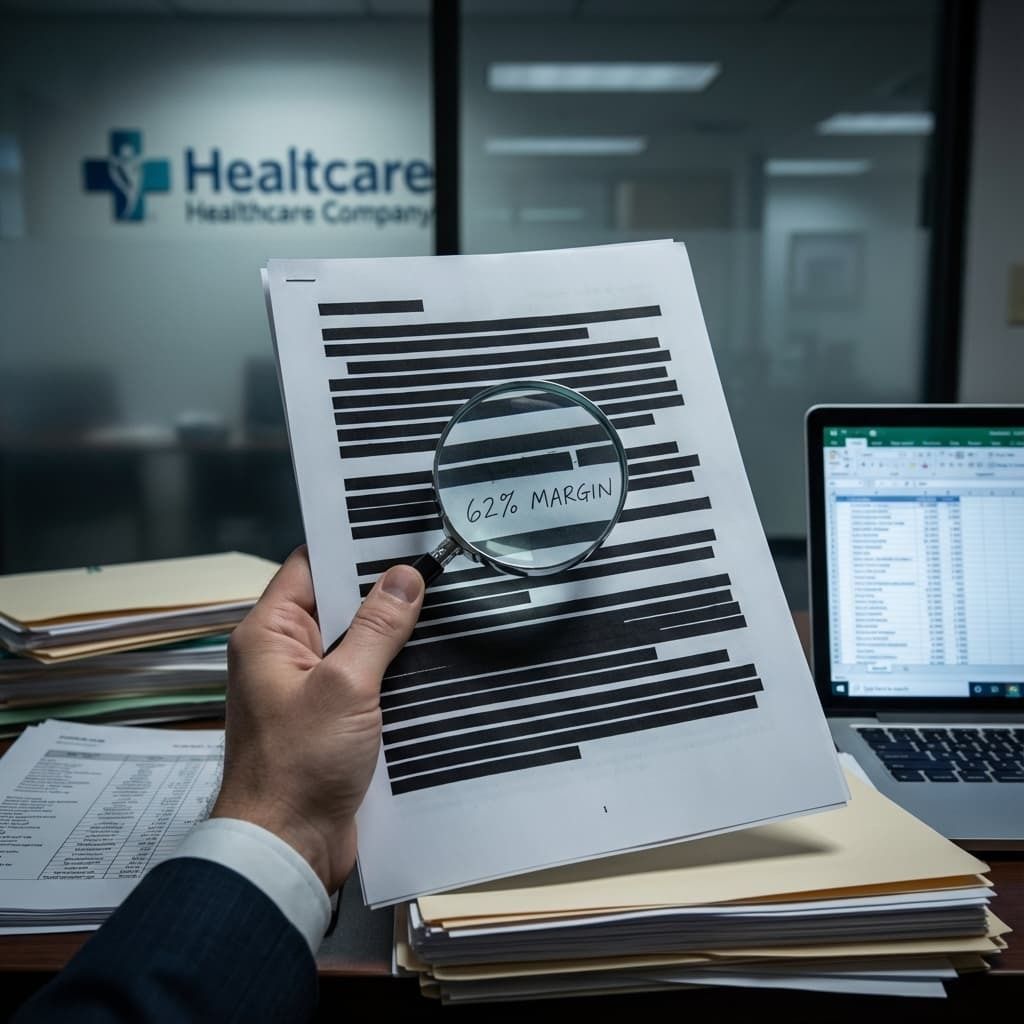
Anthem Blue Cross and Blue Shield charged the Federal Employees Health Benefits Program $39 million in subrogation fees through its subsidiary Carelon. The Office of Inspector General found a 62% profit margin on what should have been a cost-based administrative function.
That margin tells you everything about how the game works.
The Mechanics of Subsidiary Arbitrage
Insurance companies must spend 85% of premium dollars on medical care under the Affordable Care Act's medical loss ratio requirements. Anthem found the workaround.
The company reclassified administrative fees as medical claims. Subrogation recovery—the process of recouping costs from third parties after paying a claim—became "medical spending" when Carelon, Anthem's wholly owned subsidiary, charged percentage-based fees instead of negotiated administrative costs.
When you own both the insurer and the service provider, you pay yourself. Those payments count as medical expenses for compliance purposes while generating profit on the subsidiary side. The parent company satisfies regulatory requirements. The subsidiary books revenue. Consolidated profits increase.
UnitedHealth Group operates 2,694 subsidiaries using this exact model. The company's internal transfers between divisions increased from $18.3 billion in 2010 to $150 billion in 2024. Nearly 60% of Optum's revenue now comes from UnitedHealthcare, the insurance arm.
UnitedHealth's net worth increased six times since the ACA passed. Premiums keep rising. That imbalance reveals intent.
Documentation Obstruction as Strategy
When auditors requested cost documentation, Anthem "inadvertently" shared an Excel spreadsheet showing Carelon's actual subrogation costs. The company then declared the data "not accurate," "not relevant," and "not responsive."
Auditors asked for a Deloitte valuation Anthem had used to justify its pricing. The company produced six heavily redacted pages from a 900-page report.
This wasn't panic. This was calculation.
Anthem refused federal IT security audits in 2013 and again in 2015 after a data breach affecting 78.8 million people, citing "corporate policy." The OIG noted it had conducted identical audits at other insurers without incident.
Withholding documentation works when enforcement lacks teeth. The benefit of extraction exceeds the cost of resistance. Contract complexity provides legal cover. The fine print becomes a shield against oversight.
The Accidental Discovery Problem
The OIG audit appeared routine. The subrogation scheme emerged only after auditors noticed irregularities in recovery fees being passed through the plan.
Discovery was incidental, not targeted.
The Federal Employees Health Benefits Program operates as a $70 billion annual program covering eight million people. This $44 million violation surfaced through sampling that happened to include the right data points.
If this scheme ran successfully until someone looked at the right sample, how many similar practices operate undetected? The audit examined subrogation specifically but left unanswered what the numbers would look like across all Carelon services, all recovery functions, all pharmacy operations.
Routine sampling failures suggest fraud rates exceed what limited audits can detect. The contracts are written to insulate organizations from discovery. Opacity is engineered, not accidental.
Fuel your business brain. No caffeine needed.
Consider this your wake-up call.
Morning Brew}} is the free daily newsletter that powers you up with business news you’ll actually enjoy reading. It’s already trusted by over 4 million people who like their news with a bit more personality, pizazz — and a few games thrown in. Some even come for the crosswords and quizzes, but leave knowing more about the business world than they expected.
Quick, witty, and delivered first thing in the morning, Morning Brew takes less time to read than brewing your coffee — and gives your business brain the boost it needs to stay sharp and in the know.
Complexity as Competitive Advantage
Regulators have little visibility into transfer pricing between parent companies and their subsidiaries. No comprehensive data exists on affiliate markups or internal billing.
That information asymmetry is weaponized.
Three pharmacy benefit managers control 80% of the prescription drug market. Between 2017 and 2021, these PBMs generated $1.4 billion from spread pricing—charging clients more than they reimburse pharmacies. When pharmacies appeal reimbursement rates, 99.3% of appeals get rejected.
Mark Cuban called out Optum to publish drug pricing. The company responded that different rates exist for different clients based on different plans. The question remains: why? Why does transparency threaten a business model built on serving patients?
The complexity itself is the product. When patients call their insurance company with a problem and get transferred to another company they don't realize is owned by the same parent, that's not inefficiency. That's design.
The Precedent of Consequence-Free Violations
The Department of Justice attempted to block UnitedHealth's acquisition of Change Healthcare on antitrust grounds. The sale went through in September 2022. Eighteen months later, Change Healthcare suffered the largest health payments platform ransomware attack in U.S. history.
The Justice Department opened a new probe investigating whether UnitedHealth engaged in criminal Medicare fraud related to using home wellness visits to exaggerate seniors' poor health and boost government payouts.
Meanwhile, Congress introduces PBM transparency bills that remain stalled. Over half a dozen states enacted legislation in 2025. Legal outcomes remain uncertain. Even temporary injunctions delay implementation.
Anthem's defiance after getting caught signals what every consolidated health entity now understands: findings without enforcement are just expensive paperwork.
The fraud is worth the squeeze.
What the System Actually Optimizes For
From the inside, I saw incentives align around utilization suppression, not patient outcomes. From the outside, I learned that persistence, escalation, and exposure change behavior faster than clinical merit alone.
The system responds to pressure, not fairness.
Anthem and Carelon did not stumble into a 62% margin. That margin reflects a business model built on denial, delay, opacity, and exhaustion. Documentation obstruction serves a purpose. Every missing form, shifting requirement, and vague rationale increases the chance that a patient or provider stops pushing.
People resist this truth because accepting it forces a harder conclusion. Appeals alone do not fix structural misalignment. Transparency alone does not correct profit-driven friction. Good intentions inside broken incentives still produce harm.
The system does not fail patients by accident. It succeeds by design.
Understanding that truth shifts patients from passive participants to informed challengers. You stop asking for permission and start creating leverage. You document for appeal, not approval. You escalate early. You involve regulators, employers, media, and external review.
You treat access as a negotiation with power dynamics, not a benevolent process.
That knowledge changes the dynamic.


