From The Desk of

Matt dives into a specific healthcare topic to help those in the industry, and those outside of it, better understand the market drivers causing today’s healthcare challenges.
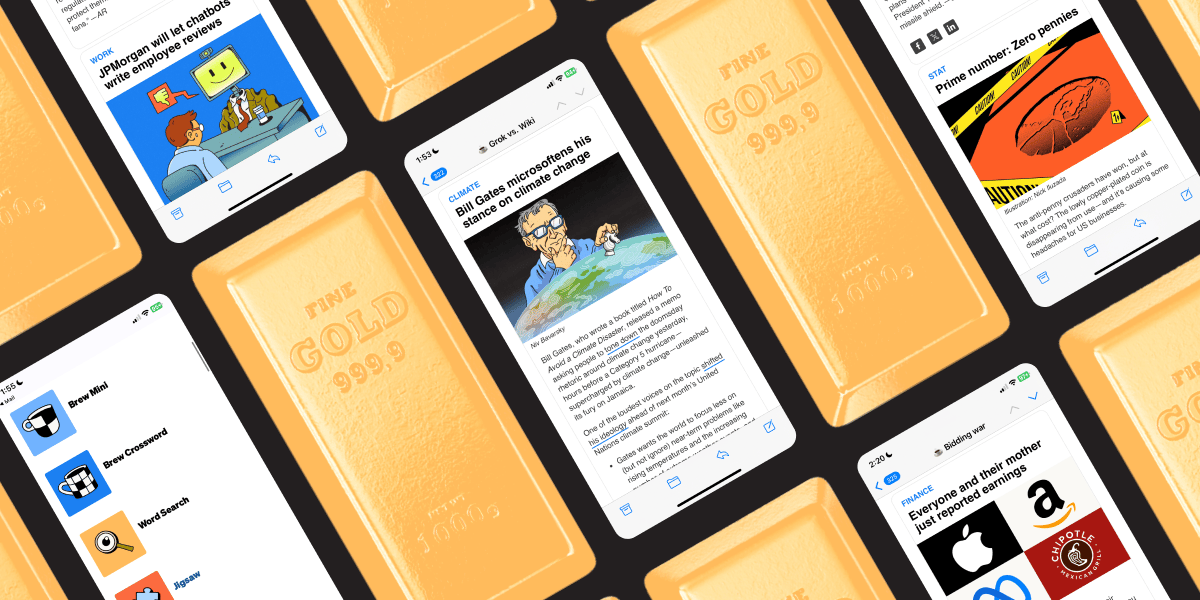
Business news worth its weight in gold
You know what’s rarer than gold? Business news that’s actually enjoyable.
That’s what Morning Brew delivers every day — stories as valuable as your time. Each edition breaks down the most relevant business, finance, and world headlines into sharp, engaging insights you’ll actually understand — and feel confident talking about.
It’s quick. It’s witty. And unlike most news, it’ll never bore you to tears. Start your mornings smarter and join over 4 million people reading Morning Brew for free.

Scrubbing language to just get the opportunity to press on…
The National Institutes of Health now forces researchers to scrub terms like "equity" and "disparities" from grant applications to secure funding. Scientists sanitize their language, hoping political appointees approve their work.
This looks new. It feels urgent. But pharma has run this playbook for years.
The pattern is identical. Researchers at NIH remove words that make decision-makers uncomfortable. Pharma companies remove patients from rooms where decisions get made. Both claim they care about the populations they exclude. Both prioritize institutional comfort over scientific reality.
Short Term Ease, Long Term Pain
I see the NIH making decisions without thinking through implications. When you exclude diverse patient populations from research, you cannot claim your products work for everyone. This matters more as we move into gene therapies and precision medicine.
Pharma faces the same problem. Companies bring patients into conversations at Phase 3, after they lock in endpoints, inclusion criteria, and trial site locations. By then, every major decision that determines whether the trial reflects patient reality is already made.
The cost shows up later. Protocol amendments run $350,000 or more per change. Recruitment delays cost up to $8 million per day. These numbers exist because companies skip the conversation that matters most.
What Gets Missed When Patients Aren't at the Table
Patient advocacy functions receive 1.6% of annual revenue at pharma and biotech companies. Direct-to-consumer advertising gets 16-18%. That gap reveals where companies think trust lives.
When you exclude patient advocacy from early clinical development meetings, you miss critical elements. Trial site locations that ignore where patient populations actually live. Lead physicians who look nothing like the patients they treat. Inclusion and exclusion criteria built without understanding disease state, comorbidities, or patient reality.
You also miss the educational materials that speak to patients in words that matter to them.
I worked with one ultra-rare disease where leadership wanted to cure the condition. That would have taken decades and millions of dollars. The patient community wanted treatment for seizures their children faced every day. Nobody had asked them. The company would have wasted years chasing the wrong goal.
The Resistance to Patient Voice
Most senior executives do not understand the value of patient advocacy functions. They do not see the point of engaging patients in clinical development discussions because it has never been part of the process.
Adding patient input feels novel. That is the problem.
Advocacy functions need more than budget increases. They need authority. They need the right to speak first in meetings about anything that impacts patients. They need veto power over protocols that ignore patient reality.
This represents a power shift. When advocacy speaks first, the entire conversation changes. Medical leaders and corporate executives can no longer make decisions in isolation and bring patients in later to validate choices already made.
The Data Makes the Case
A $100,000 patient engagement exercise only needs to reduce amendment probability by 0.1% to justify its cost. For a pre-Phase 2 project, avoiding one protocol amendment and improving enrollment increases net present value by $62 million.
The reduction in development cost from one less amendment exceeds engagement costs by a factor of 5 for pre-Phase 2 and 21 for pre-Phase 3.
Advocacy leaders need to use this data. Point to facts showing patients expect involvement early. Show medical teams the barriers they have faced historically. Get regulatory teams to acknowledge their challenges. Everyone knows the problems exist in clinical development. The question is whether anyone will admit it.
What Happens When We Don't Fix This
Therapies get approved for populations never included in study populations. Those patients will not benefit from approved therapies. Certain demographics remain excluded from healthcare. Distrust of the medical system continues to grow.
The NIH situation and pharma's operational blind spots create the same outcome. Populations get systematically excluded. Research becomes less valid. Trust erodes further.
Fight Like Hell
Patient advocacy leaders need to fight for awareness of their ability to connect with patient populations. Fight for recognition of the ROI from engaging patients early. Fight for acknowledgment of the impact on the business bottom line when advocacy succeeds.
Advocacy cannot remain a bystander function in pharma and biotech organizations. The role demands leadership that organizations and patients need.
When advocacy functions finally get real about barriers everyone has faced, something shifts in the room. Nobody has to pretend problems will not exist in the future. Teams can focus on challenges they have encountered and work with patient communities to prevent them.
That moment brings what every clinical development meeting needs. Hope and passion for patient outcomes.
The NIH is sanitizing language under political pressure. Pharma sanitizes patient input under operational convenience. Both choices cost lives. Both can change.
The question is whether advocacy leaders will claim the authority they need to make that change happen.
Thank you for reading! If you get the chance, don’t miss out on Matt’s TEDx talk informing the general public on the value of a patient advocate and how patient’s never have to go through healthcare struggles alone!